Team M. LAFFARGUE
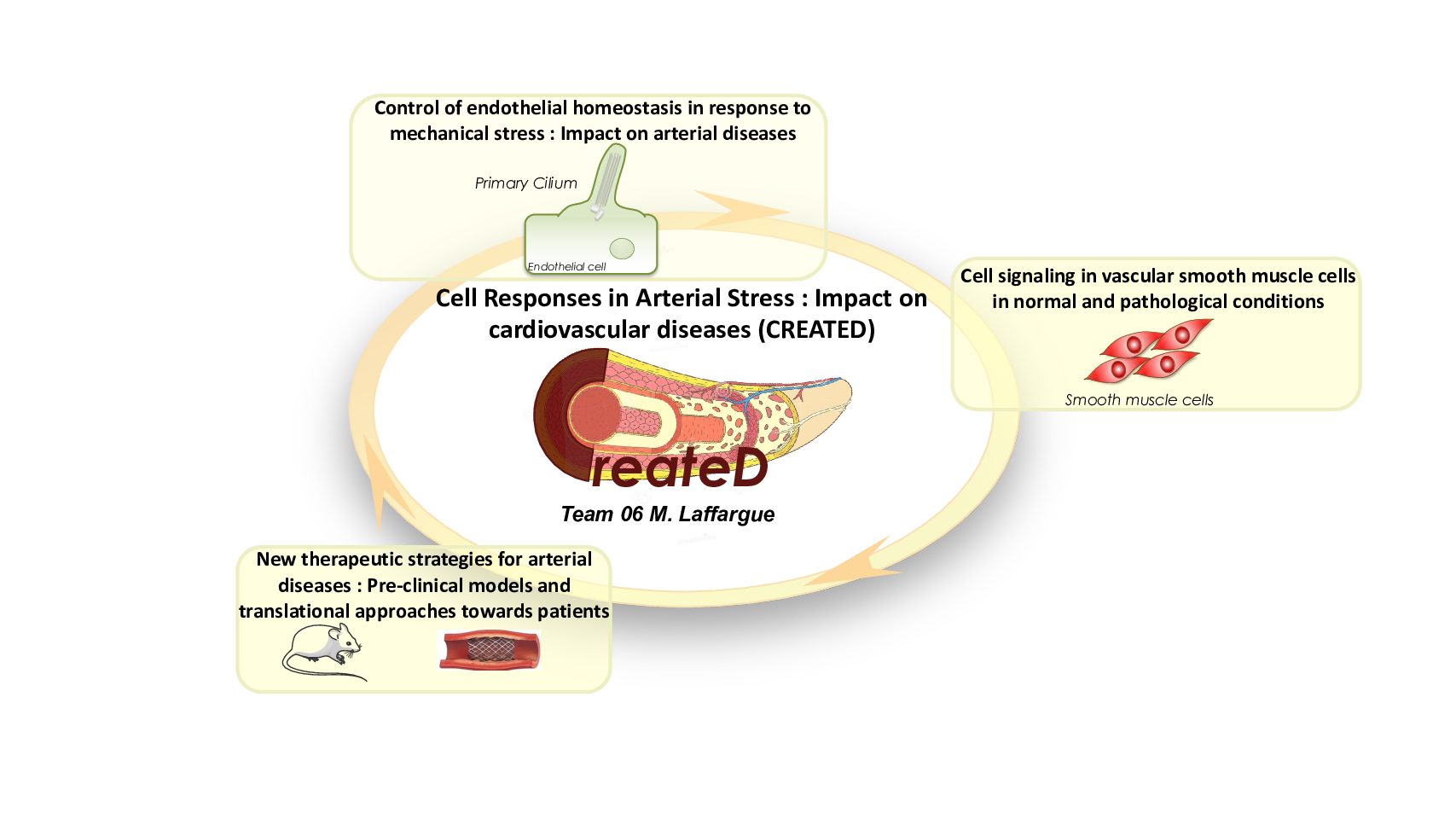
Cell Responses in Arterial Stress : Impact on cardiovascular diseases (CREATED)
Our team groups together experts in cell signalling dedicated to the understanding of molecular mechanisms involved in vascular homeostasis (PI3K/mTOR pathways) and modulated by various stresses in pathologic conditions or related to aging (mechanical, oxydative or metabolic stresses, inflammation). In collaboration with clinicians from the hospital Toulouse Rangueil, we develop original pre-clinical models of arterial lesions with the aim to improve actual treatments of atherosclerosis and the prevention of transplant vasculpathies causing organ rejection.
Team members

Muriel LAFFARGUE

Nathalie AUGE

Stéphanie GAYRAL

Damien RAMEL

Natalia Smirnova

Caroline CAMARE

Anne Darmon

Serena GIUNTINI

Isra MENTOURI

Laura Mickiewicz

Nicole MALET

Anne NEGRE-SALVAYRE

Robert SALVAYRE

Didier CARRIE
Kevin CORMIER

Arnaud DEL BELLO

Nicolas CONGY-JOLIVET
Control of endothelial homeostasis in response to mechanical stress : Impact on arterial diseases

Coordinators : Stéphanie GAYRAL, Caroline CAMARE, Anne NEGRE-SALVAYRE, Muriel LAFFARGUE
Environnemental hemodynamic milieu controls endothelial cell activation and their maintenance of their barrier function. Study of the perturbations of mechanosensors able to integrate these bio-mechanics stimuli and their associated signalling pathways associated with pathological conditions, will allow us to propose new therapeutic avenues to prevent endothelial dysfunction.
Cell signaling in vascular smooth muscle cells in normal and pathological conditions
Coordinators : Nathalie AUGE, Damien RAMEL, Natalia SMIRNOVA, Anne NEGRE-SALVAYRE, Muriel LAFFARGUE
Smooth muscle cells are at the center stage of the arterial responses in normal and pathological conditions. We investigate their signaling pathways to decipher the molecular mechanisms leading to their deregulation found in cardiovascular diseases such as atherosclerosis or explant rejection but also in disturbed metabolic conditions such as diabetes.
Transplant vasculopathy : Pre-clinical models and translational approaches towards patients

Coordinators : Natalia SMIRNOVA, Arnaud DEL BELLO, Anne NEGRE-SALVAYRE, Didier CARRIE, et Muriel LAFFARGUE
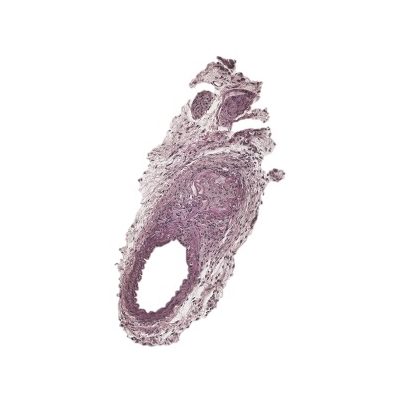
With the aim to test new therapeutic strategies to prevent vascular damages, we have developed original mice models of arterial lesions (mechanical injury of carotids, humanized model of aorta transplantation) found in cardiovascular diseases and in transplant vasculopathies. In collaboration with industrial partners and clinicians, we plan to test various chemicals compounds targeting PI3K/mTOR signaling pathways in these pre-clinical models and eventually develop a translational approach towards patients.
SELECTED PUBLICATIONS
Ticagrelor promotes arterial healing and shows superiority to clopidogrel in preventing neoatherosclerosis.
A minor tweak in transplant surgery protocols alters the cellular landscape of the arterial wall during transplant vasculopathy.
PI3KCIIα-Dependent Autophagy Program Protects From Endothelial Dysfunction and Atherosclerosis in Response to Low Shear Stress in Mice.
Smooth muscle cells-derived CXCL10 prevents endothelial healing through PI3Kγ-dependent T cells response. Cardiovasc Res. 2020. Pubmed
PI3KC2α-dependent and VPS34-independent generation of PI3P controls primary cilium-mediated autophagy in response to shear stress. Nat Comm. 2020. Pubmed


Inserm/UPS UMR 1297 - I2MC Institut des Maladies Métaboliques et Cardiovasculaires
1 avenue Jean Poulhès - BP 84225 - 31432 Toulouse Cedex 4
Tél. : 05 61 32 56 00
Horaires
Du lundi au vendredi
8h30 - 12h30 / 13h45 -16h45






